For decades, doctors have used electrical pulses to help people with Parkinson’s disease manage symptoms like tremors, stiffness, and slow movements. This technique, known as deep brain stimulation (DBS), has been life-changing for some patients, but for others, it hasn’t worked as well or has caused unwanted side effects.
Musumeci Online – The Podcast. It is perfect for driving, commuting, or waiting in line!
Now, an advanced version of the technology—called adaptive deep brain stimulation (aDBS)—is bringing new hope. Similar to how a smart thermostat adjusts the temperature based on the weather, aDBS continuously monitors brain activity and fine-tunes electrical pulses in real time. This personalized approach makes the treatment more effective, precise, and efficient.
What is Deep Brain Stimulation?
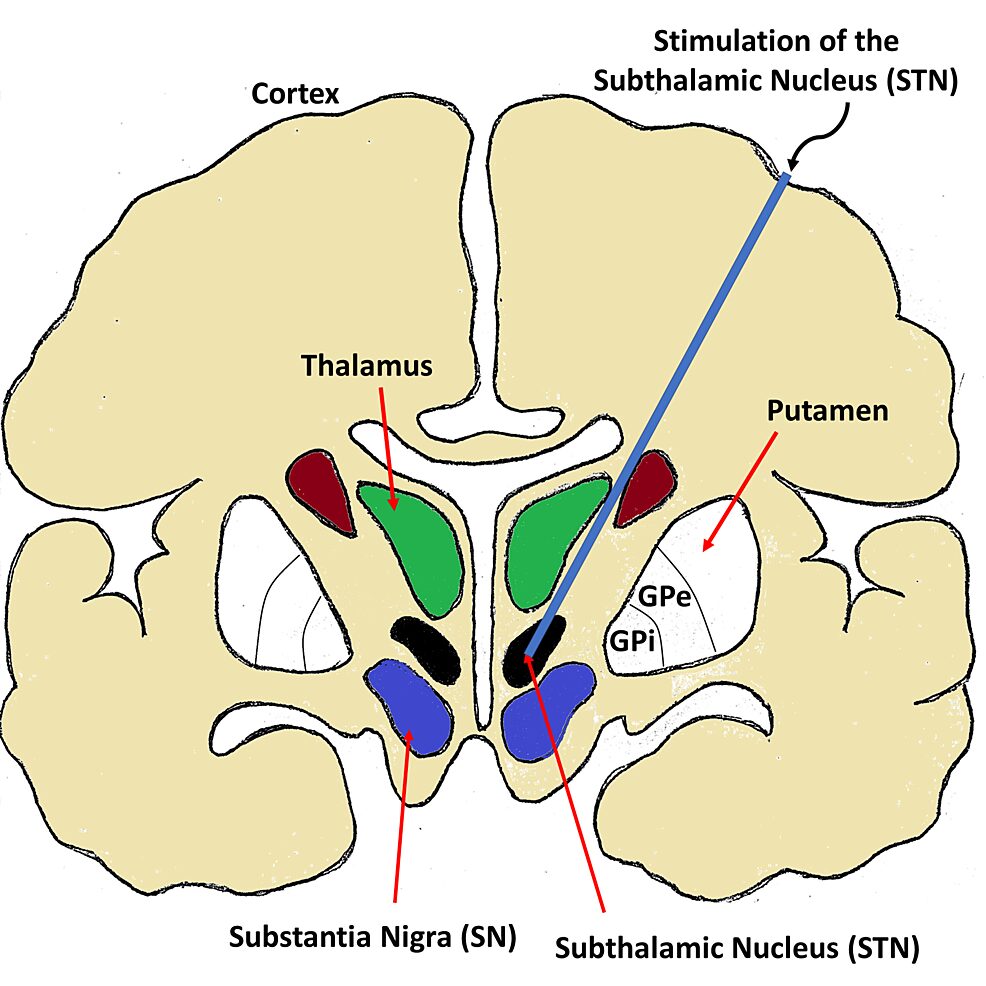
Imagine a pacemaker, but for the brain instead of the heart. Traditional DBS involves implanting electrodes into specific areas of the brain that are affected by Parkinson’s. These electrodes are connected to a small device placed under the skin of the chest, which sends electrical signals to help regulate brain activity.
However, until recently, these signals were delivered at a constant rate, whether the brain needed them or not. It’s like having a light that stays on all day, even when the sun is shining. This “one-size-fits-all” approach worked for some patients but was far from perfect.
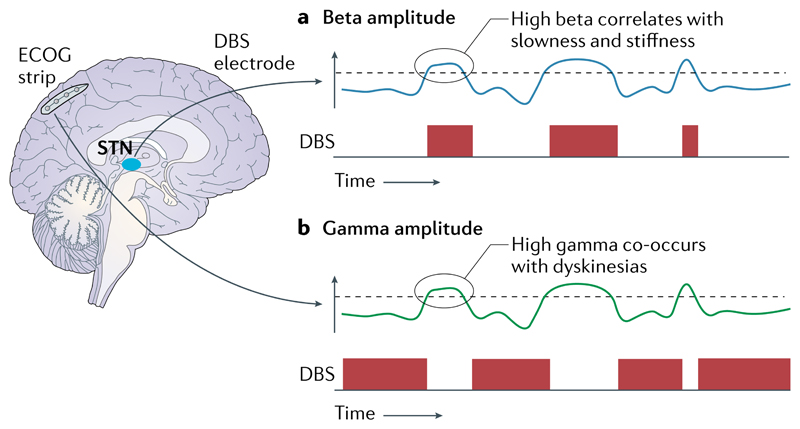
With aDBS, the system becomes smarter. It listens to the brain’s natural signals and only activates when necessary—similar to how modern heart pacemakers adjust their pacing based on a person’s heart rate. This means fewer side effects and better symptom control, as the stimulation is tailored to the patient’s real-time needs.
The Science Behind aDBS
Parkinson’s disease disrupts the brain’s ability to coordinate movement, partly due to abnormal beta waves—patterns of electrical activity in the brain. Traditional DBS helped by sending a steady stream of electrical signals to suppress these waves. However, Parkinson’s symptoms fluctuate throughout the day based on medication, activity levels, and disease progression. A constant signal can’t adapt to these changes, making treatment less effective at times.
With aDBS, the device continuously tracks beta waves and adjusts its signals accordingly. Instead of completely blocking beta waves, it keeps them within a healthy range, making the treatment more natural and efficient.
How Did This Breakthrough Happen?
Dr. Helen Bronte-Stewart and her team at Stanford University have spent years studying how movement and brain activity are connected. By analyzing brain signals from Parkinson’s patients with implanted DBS devices, they identified the most critical abnormal patterns to target.
The idea of using real-time brain monitoring to personalize treatments represents a major shift in medicine. It’s an exciting step forward
Early experiments in 2015 used smartwatches to monitor tremors and adjust DBS settings. This eventually led to today’s aDBS technology, which directly tracks beta waves inside the brain for even greater precision. Thanks to this research, the U.S. Food and Drug Administration (FDA) has now approved aDBS, making it available to many more patients in the U.S. who already have compatible DBS devices.
What’s Next for aDBS?
This is just the beginning. With FDA approval, more people with Parkinson’s will have access to aDBS, and researchers will continue refining the technology to make it even more effective. In the future, this approach could also be applied to other neurological conditions, like epilepsy or severe depression.
The idea of using real-time brain monitoring to personalize treatments represents a major shift in medicine. It’s an exciting step forward, not just for Parkinson’s patients, but for the future of neuroscience and brain-computer interfaces.

Leave a Reply